Simple clinical tool can help diagnose spinal fractures in people with osteoporosis
A Keele researcher has played a key role in the development of a new tool to help clinicians diagnose spinal fractures in osteoporosis patients.
Currently only one in three patients are diagnosed with broken bones in the back due to osteoporosis, due in part to medical staff finding it difficult to know who should have a back X-ray.
To help address this important diagnostic care gap, a research team led by the University of Bristol have developed an online clinical checklist called Vfrac, to help medical staff spot vertebral fractures that might otherwise have been missed, with the goal of ensuring more older women with vertebral fractures are diagnosed.
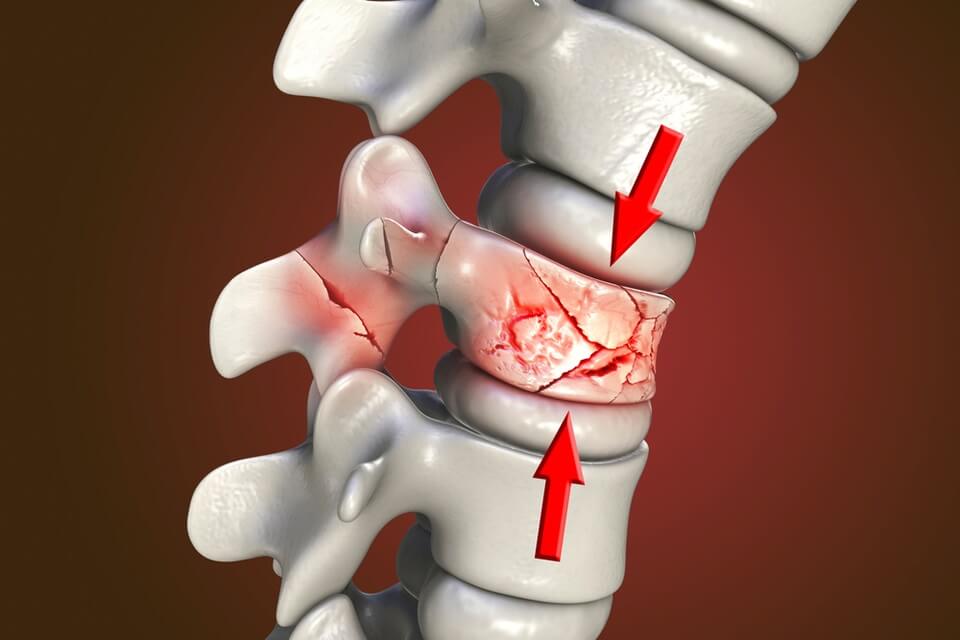
Nearly three million people in the UK have osteoporosis, which is one of the most common musculoskeletal conditions in older people. Osteoporotic vertebral fractures (broken bones in the back due to osteoporosis) are particularly important because they identify people at high risk of future fractures.
This study, published in Age and Ageing and funded by Versus Arthritis, also sought to identify whether the tool could help clinicians make more accurate predictions based on patients’ self-reported back pain, and assess the tool’s potential cost-effectiveness for use in the NHS.
The Vfrac cohort study recruited 1,635 women over the age of 65 with self-reported back pain in the previous four months, from nine GP practices in Bristol and 13 GP practices in Stoke-on-Trent.
Participants from Stoke played a huge role in the study, with over 1,000 of the women involved being recruited from the local area.
Participants completed questionnaires and underwent a physical examination, to assess them for common risk factors for osteoporosis such as previous fragility fractures, smoking, and use of steroid tablets.
The researchers found that over 70 per cent of people with vertebral fractures were diagnosed correctly using the Vfrac checklist, a significant improvement compared to the current 30 per cent of patients who currently receive a correct diagnosis.
Dr Zoe Paskins from Keele’s School of Medicine co-authored the research, and said: “This research is a really important step forward in helping to increase early and accurate diagnosis of spinal fractures.”
Lead author Emma Clark, Professor of Clinical Musculoskeletal Epidemiology at the University of Bristol, and Consultant Rheumatologist at North Bristol NHS Trust (NBT) added: “Vfrac can help healthcare practitioners decide which older women attending their GP with back pain are at high risk of currently having one or more broken bones in the back due to osteoporosis and need a diagnostic spine X-ray.
“Our study found approximately one third of people recommended to have X-rays by Vfrac will have a vertebral fracture. Vfrac identified more than 90 per cent of those with severe vertebral fractures and approximately two-thirds of those with mild or moderate fractures. We now want to test Vfrac in a real-world clinic.”
Most read
- Astronomer from Keele helps take the first close-up picture of a dying star outside our galaxy
- Keele University signs official partnership with Cheshire College South & West
- Keele partners with regional universities to tackle maternity inequalities across the West Midlands
- Keele Business School MBA ranks in Top 40 for sustainability in prestigious global ranking
- Keele trains next generation of radiographers using virtual reality in regional first
Contact us
Andy Cain,
Media Relations Manager
+44 1782 733857
Abby Swift,
Senior Communications Officer
+44 1782 734925
Adam Blakeman,
Press Officer
+44 7775 033274
Ashleigh Williams,
Senior Internal Communications Officer
Strategic Communications and Brand news@keele.ac.uk.

