Parents want the HPV vaccine for their sons – new research

Human papillomavirus (HPV) is a sexually transmitted infection that causes diseases that affect both men and women. In the UK, girls are vaccinated against HPV but boys are not.
There are more than 100 types of HPV. Two of the low risk types (six and 11) cause more than 90% of genital warts. Other high risk types of HPV (especially 16 and 18) can cause cervical, vulval, vaginal, head, neck and throat, anal and penile cancers. While the incidence of cervical cancer in the UK has fallen since the 1990s, thanks to the NHS cervical screening programme, the incidence of those cancers that affect both men and women is on the rise.
More than 80% of sexually active people will be exposed to HPV in their lifetime. Genital HPV infection is spread during sexual intercourse and skin-to-skin contact of the genital areas. Wearing a condom reduces the risk of infection but does not provide complete protection. Once a person has been infected, their immune system will fight the virus and, in most cases, the virus will have no ill effects. But, for some people, the virus will progress to cause warts or cancer.
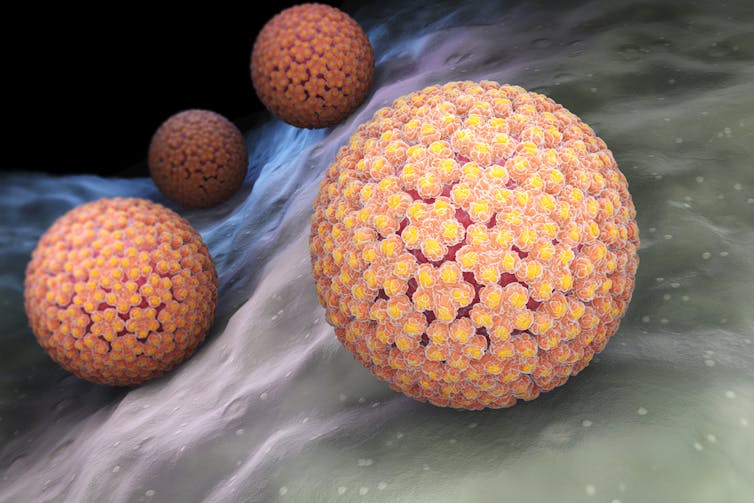
HPV causes a range of cancers, including cervical, penile, anal and throat cancer. Tatiana Shepeleva/Shutterstock.com
Since 2008, 12- and 13-year-old girls in most of the UK (11 to 13 in Scotland) have been offered the chance to be vaccinated against HPV via a school-based programme. In a phased rollout from April 2018, men aged 45 or younger who have sex with men will be offered the HPV vaccination in England at sexual health clinics and HIV clinics, bringing England in line with the rest of the UK. But boys are not likely to be offered the HPV vaccine any time soon.
Too little, too late
One rationale for not vaccinating boys is that if enough girls are vaccinated (currently, around 85% of girls have the necessary two doses in England), this provides “herd immunity” to men, meaning that if women don’t have the virus, men will not be able to catch it either.
The main problem with the herd immunity argument, when it is girls rather than boys who are vaccinated, is that it doesn’t provide protection for men who have sex with men, or for men who have sex with unvaccinated women – for example, women from countries without a vaccination programme, or women who are too old to have been eligible for the vaccination.
Men who have sex with men are particularly vulnerable to HPV-related anal cancer. Although they can now opt to have the vaccination, it is too little, too late.
The HPV vaccination is most effective when it is given before exposure to the virus (before sexual activity starts), and also when it is given before puberty, when immune systems are able to provide a stronger antibody response.
Gender-neutral vaccination has wide support among the medical community with professional organisations such as the British Dental Association and The Faculty of Public Health favouring vaccination for both boys and girls.
Survey results
It is not just professionals who want to see the vaccination extended to boys. A recent Wellcome-funded survey of 186 parents of teenage boys in North Staffordshire that we conducted found that many of the parents were not aware of the health consequences of HPV for men. The research, published in PLOS ONE, revealed that once they were provided with this information, however, most parents wanted the vaccine to be available to their sons.
![]() Several countries vaccinate both girls and boys against HPV, including the US, Canada, Austria, Australia and New Zealand. It is unacceptable, as society strives for equality in so many areas, that the UK should not extend the protection afforded by the HPV vaccination to boys as well as girls.
Several countries vaccinate both girls and boys against HPV, including the US, Canada, Austria, Australia and New Zealand. It is unacceptable, as society strives for equality in so many areas, that the UK should not extend the protection afforded by the HPV vaccination to boys as well as girls.
Sue Sherman, Senior Lecturer in Psychology, Keele University
This article was originally published on The Conversation. Read the original article.
Most read
- Keele University partners with Telford College and NHS to teach new Nursing Associate apprenticeship in Shropshire
- Emotion aware chatbot developed by Keele scientists offers transformative potential for mental health care
- First study of its kind sheds new light on Britain’s ‘forgotten’ World War Two decoy sites
- Keele cardiologist travels to Ethiopia to improve care for heart patients
- Keele academic wins prestigious prize for short story set in Stoke-on-Trent
Contact us
Andy Cain,
Media Relations Manager
+44 1782 733857
Abby Swift,
Senior Communications Officer
+44 1782 734925
Adam Blakeman,
Press Officer
+44 7775 033274
Ashleigh Williams,
Senior Internal Communications Officer
Strategic Communications and Brand news@keele.ac.uk.


